Malnutrition Care Score (MCS)
In the United States, quality measures help patients choose high-performing clinicians and enable healthcare providers to assess and improve care. The Malnutrition Care Score (MCS) - formerly the Global Malnutrition Composite Score (GMCS)—is the first nutrition-focused electronic clinical quality measure (eCQM) included in the Centers for Medicare and Medicaid (CMS) Hospital Inpatient Quality Reporting (IQR) Program under the FY 2023 Inpatient Prospective Payment System (IPPS) Final Rule. Developed and stewarded by the Academy of Nutrition and Dietetics and the Commission on Dietetic Registration (CDR), the MCS was endorsed by the National Quality Forum (NQF) Consensus Standards Approval Committee (CSAC) for 2021-2024. In Spring 2024, the Partnership for Quality Measurement (PQM) Endorsement and Maintenance (E&M) Committee also endorsed updated specifications that include the expansion to adults aged 18 and older.
- What are Quality Measures?
- What is the Malnutrition Care Score?
- The Value of Implementing a Malnutrition Quality Measure
- Free Education Resources
- MCS Implementation Resources
- References and Additional Peer-Reviewed Documents
The Centers for Medicare and Medicaid Services (CMS) collect and analyze data to produce reports utilizing quality improvement and quality measurement data to improve outcomes while reducing burden on clinicians and providers.
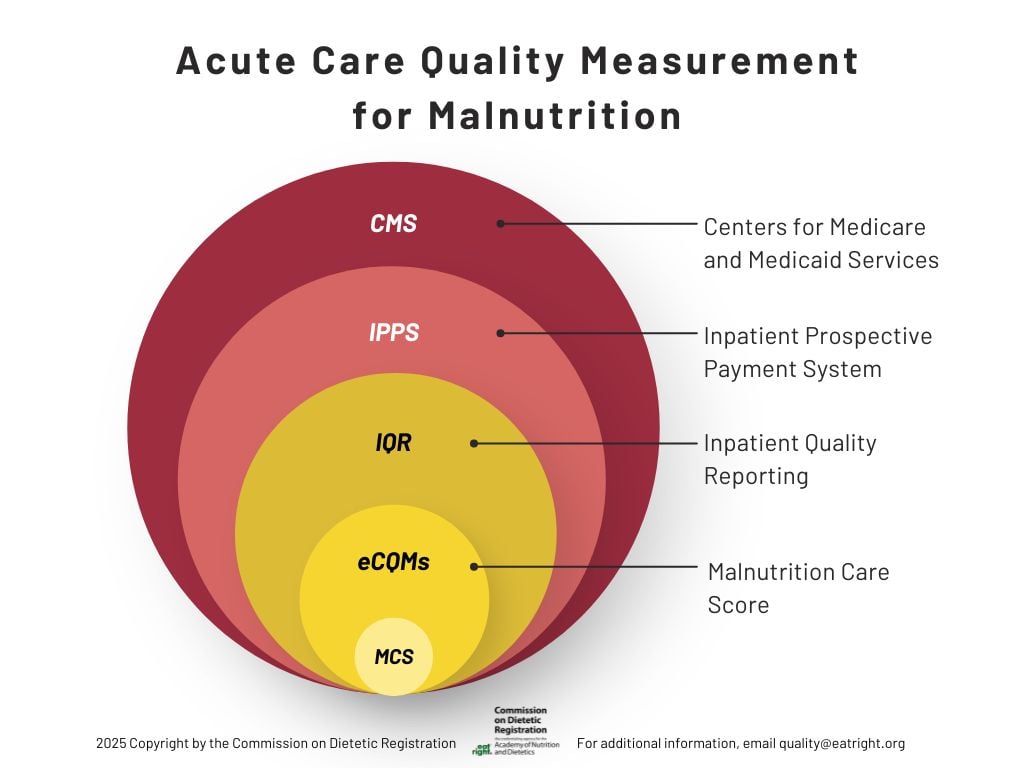
Within the CMS programs lies the Inpatient Quality Reporting (IQR) Program, a pay-for-reporting initiative that requires hospitals to submit quality and safety data to reduce complications, lower mortality rates, and deliver high-quality care. These results are publicly shared on the Care Compare website.
Electronic clinical quality measures (eCQMs), part of the IQR Program, leverage data extracted from electronic health records (EHR) or health information technology (HIT) systems to assess care quality. Hospitals submit eCQM data directly from these systems.
For Reporting Period 2024-2025, Eligible Hospitals and Critical Access Hospitals must report on 6 electronic clinical quality measures for each reporting period-three mandatory and three self-selected. The MCS was approved as a self-selected eCQM and is 1 of 11 eCQMs available for reporting period 2026 and beyond.
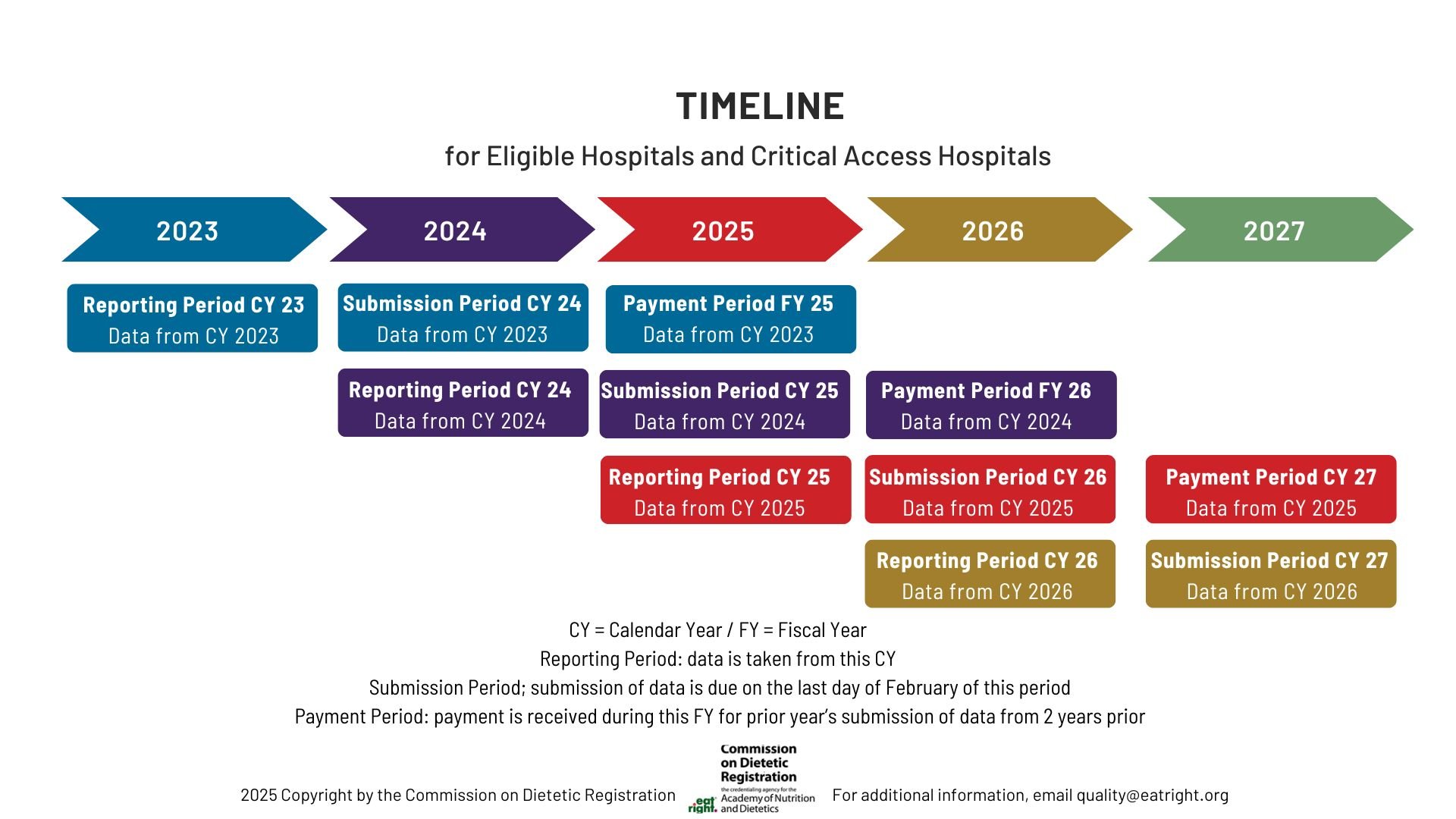
When implementing the MCS, understanding key reporting terms is crucial. The Reporting Period is the calendar year that the data will be collected. The data collected will then be submitted the following year, during the Submission Period. Ultimately, the data reported and submitted will directly be linked to the Payment Period Fiscal year that corresponds to the year after the Submission Period.
The MCS assesses the percentage of hospitalizations for adults 65 years and older (if reporting data from 2024 and 2025) or all adults 18 year of age (for reporting data in 2026 or later), with a length of stay of at least 24 hours that have received optimal malnutrition care during the current inpatient hospitalizations.
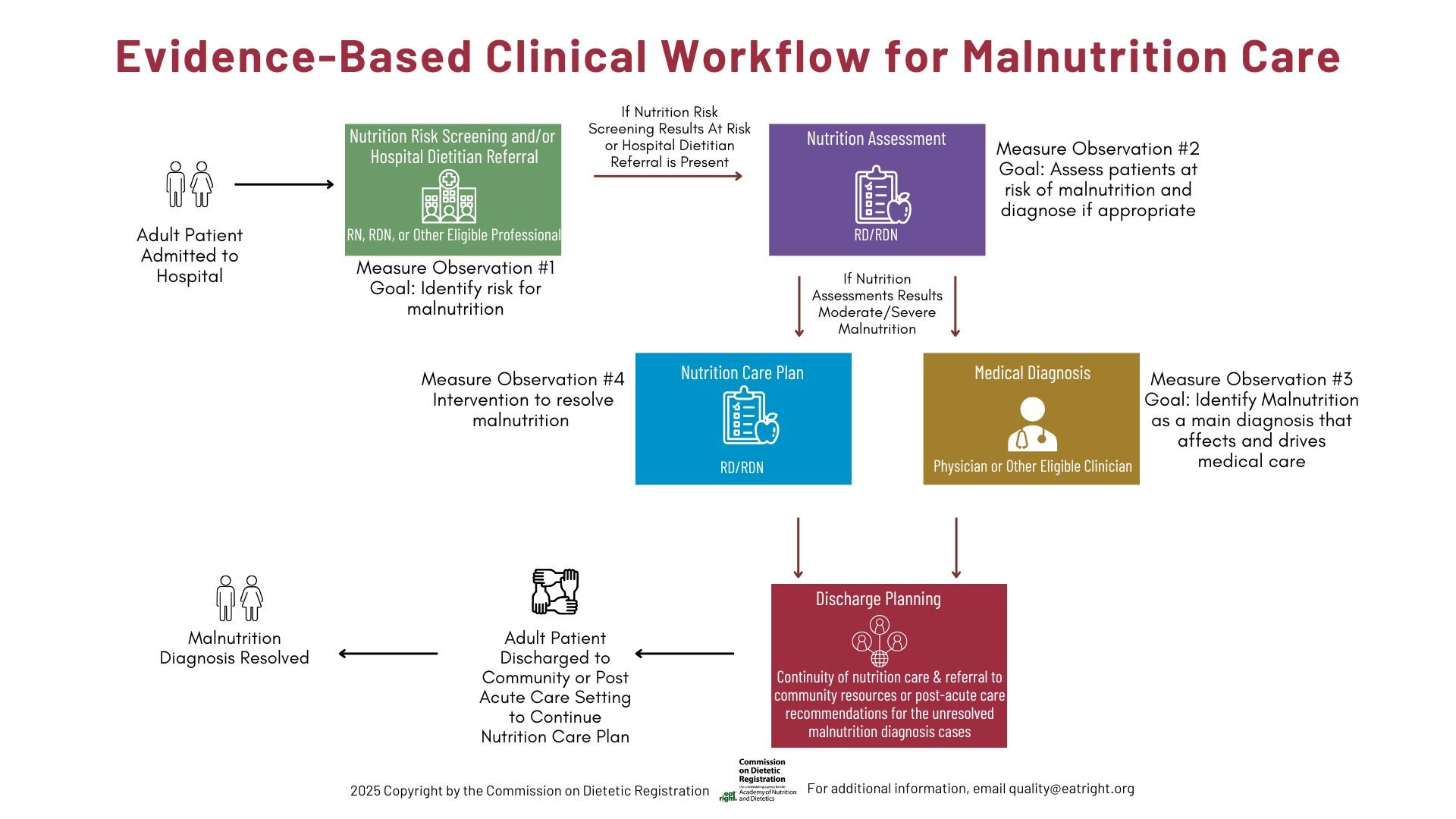
The MCS follows evidence-based guidance to support malnutrition care, as shown below.
For measure specifications and implementation tools go here.
Malnutrition is defined as the inadequate intake of nutrients or energy, over time, and can have many root causes. A hospitalized patient with malnutrition can place a strain on resources, and negatively affect quality outcomes, as shown in the figure below.
Clinical guidelines for addressing malnutrition in acute care settings establish that a patient should first be screened for risk for malnutrition, those at risk should be further assessed, and if found to have malnutrition by assessment, then a nutrition support plan should be established (3).
Effective malnutrition care processes benefit from interdisciplinary collaboration. This type of care offers an opportunity to develop a comprehensive and individualized assessment and treatment plan, and thus supporting accurate diagnosis and effective care. The following graphic shows the key roles different profession in a hospital can offer to help achieve successful implementation of the MCS.
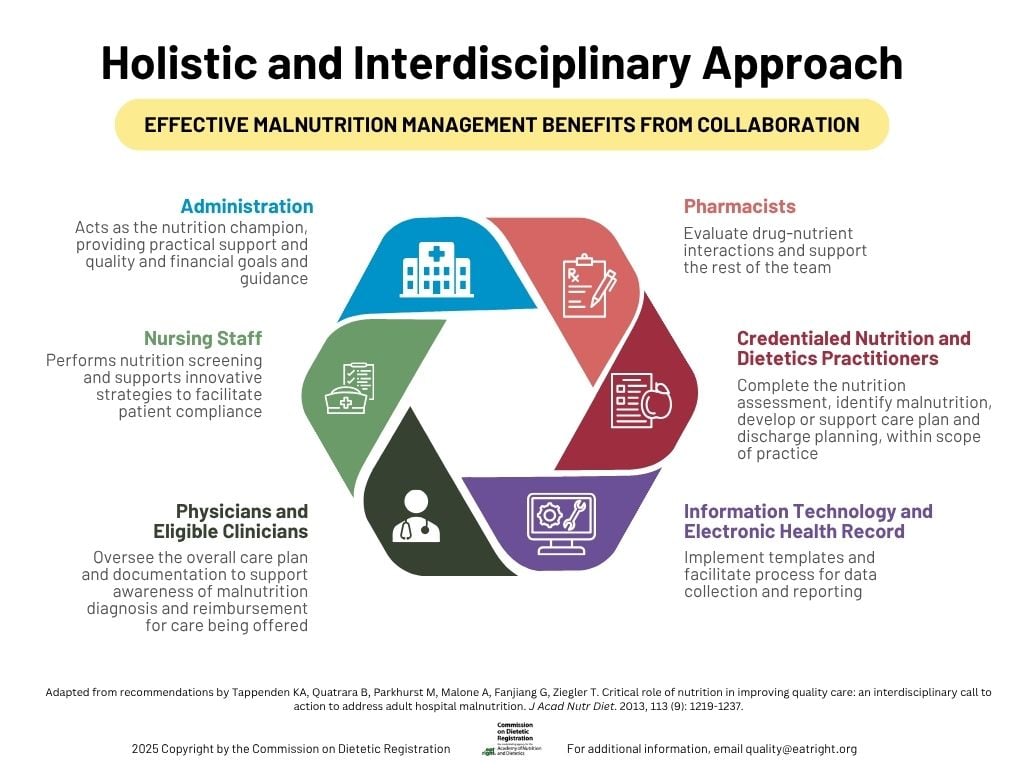
The MCS follows the recommended workflow of evidence-based malnutrition care and encourages interdisciplinary care discussions and involvement during implementation and clinical care. Although the MCS was developed for the acute care setting, its proven framework can be adapted to any practice area to improve patient outcomes and quality of care.
Benefits of implementing the MCS:
- Providing care measured through the MCS supports hospitals’ strategic plans to address social determinants of health and equity.
- All four components are often already established in acute care facilities.
- Addresses several clinical areas or quality indicators simultaneously, including:
- Nutrition Screening - The Joint Commission
- Social Determinants of Health and Food Insecurity - The Joint Commission, CMS, 2023 Healthcare Effectiveness Data and Information Set’s (HEDIS) Social Need Screening and Intervention Measure
- Health Equity Advancement - identified by CMS as a priority eCQM
- Rural Health Improvement- identified by NQF as a key measure**
- Combines several quality measures into one single composite score, giving a more comprehensive picture of clinical care than a single measure.
- Promotes multidisciplinary engagement, supporting communication and employee satisfaction efforts.
- Malnutrition Quality Improvement Initiative (MQii): a project of the Academy of Nutrition and Dietetics, Avalere Health, and other stakeholders who collaborate to provide guidance and expertise for clinical malnutrition.
- MQii Toolkit: supports the implementation of malnutrition care best practices.
- MQii Learning Collaborative, a community of clinicians committed to improving delivery of malnutrition care in hospitals and health systems across the US.
- Reports:
- Dialogue Proceedings for Advancing Patient-Centered Malnutrition Care Transitions
- Roundtable Proceedings for Advancing Health Equity Through Malnutrition Quality Measurement
- Enduring activities:
- November 2023: Advancing Quality and Strengthening Interdisciplinary Collaboration (Part I) (1 free CPEU)
- Malnutrition and Health Equity: Key Measures of Quality Care for Nutrition and Dietetics Practitioners (2.75 CPEUs)
- Business Case for the Global Malnutrition Composite Score (GMCS) (4.5 CPEUs)
- February 2024: Value of Nutrition and Dietetics Credentialed Practitioners in Optimizing Quality Outcomes from the Interdisciplinary Team Perspective (Part II) (1 free CPEU)
- May 2024: Measuring Nutrition Practice Outcomes by Demonstrating Value in the Real World (1 free CPEU)
- July 2024: Understanding the Global Malnutrition Composite Score: Key Insights and Major Updates for Reporting Period 2025 (1 CPEU)
- Infographics:
- Peer-Reviewed Articles:
- Measuring Malnutrition and Food Insecurity to Facilitate Quality Care and Health Equity Journal of the Academy of Nutrition and Dietetics. October 2022 Supplement.
- The Updated Global Malnutrition Composite Score Clinical Quality Measure: Its Relevance to Improving Inpatient Clinical Outcomes and Health Equity. Journal of the Academy of Nutrition and Dietetics. February 2024.
- The Global Malnutrition Composite Score: Impacting malnutrition care. Nutrition in Clinical Practice. June 2024.
- Additional Resources
- Action Plan to Implement the GMCS
- August 2022: Global Malnutrition Composite Score
- August 2023: Global Malnutrition Composite Score Town Hall
- The Joint Commission Expert to Expert 2024 New Measure Review Webinar for the Global Malnutrition Composite Score eCQM
- MQii August Virtual Office Hour Session
- Click here for additional MCS or quality related resources
| Annual Update Cycle | Application Year* | Consensus Based Endorsement | Specification and Value Sets | Specification Manual | Additional Resources |
| 2023 | Reporting Period CY 2024 Submission Period CY 2025 Payment Period FY 2026 | NQF #3592e through Fall 2024 | Global Malnutrition Composite Score | eCQI Resource Center (healthit.gov) | GMCS Specification Manual | |
| 2024 | Reporting Period CY 2025 Submission Period CY 2026 Payment Period FY 2027 | PQM #3592e, Spring 2024, through Spring 2029 | Global Malnutrition Composite Score | eCQI Resource Center (healthit.gov) | AU2024 GMCS Specifications Manual | |
| 2025 | Reporting Period CY 2026 Submission Period CY 2027 Payment Period FY 2028 | PQM #3592e, Spring 2024, through Spring 2029 | Malnutrition Care Score | eCQI Resource Center | AU2025 MCS Specifications Manual |
*Reporting Period is the period where data is collected. Submission Period is when data collected the prior year is submitted, usually during the Spring Quarter. Payment Period is the fiscal year the payment could potentially be affected if criteria for reporting is met or not met.
Additional implementation resources:
For additional information, questions, or support with implementation needs, please email quality@eatright.org.
- Avalere Health. (2022). Leveraging Inpatient Malnutrition Care to Address Health Disparities. Retrieved July 27, 2023, from https://avalere.com/insights/leveraging-inpatient-malnutrition-care-to-address-health-disparities.
- Barrett ML, B. M. (2018). Non-maternal and Non-neonatal Inpatient Stays in the United States Involving Malnutrition, 2016. U.S. Agency for Healthcare Research and Quality. Retrieved July 27, 2023, from https://hcup-us.ahrq.gov/reports/ataglance/HCUPMalnutritionHospReport_083018.pdf.
- Mueller C, Compher C & Druyan ME and the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. Nutrition Screening, Assessment, and Intervention in Adults. Journal of Parenteral and Enteral Nutrition. 2011; 35 (1): 16-24. A.S.P.E.N. Clinical Guidelines (wiley.com)
- Arensberg MB, Saal-Ridpath K, Kerr K, Phillips W. Opportunities to Improve Quality Outcomes: Integrating Nutrition Care Into Medicare Advantage to Address Malnutrition and Support Social Determinants of Health. Inquiry. 2022 Jan-Dec; 59: 469580221081431. doi: 10.1177/00469580221081431. PMID: 35255728; PMCID: PMC8908402.
- Bechtold ML, Nepple KG, McCauley SM, Badaracco C, Malone A. Interprofessional implementation of the Global Malnutrition Composite Score quality measure. Nutr Clin Pract. 2023 Oct;38(5):987-997. doi: 10.1002/ncp.11033. Epub 2023 Jul 11. PMID: 37431796.
- Doley J, Phillips W. Accurate Coding Impacts the Geometric Length of Stay for Malnourished Inpatients. J Acad Nutr Diet. 2019 Feb;119(2):193-198. doi: 10.1016/j.jand.2017.10.023. Epub 2018 Feb 21. PMID: 29429855.
- Guenter P, Abdelhadi R, Anthony P, Blackmer A, Malone A, Mirtallo JM, Phillips W, Resnick HE. Malnutrition diagnoses and associated outcomes in hospitalized patients: United States, 2018. Nutr Clin Pract. 2021 Oct;36(5):957-969. doi: 10.1002/ncp.10771. Epub 2021 Sep 6. PMID: 34486169.
- Marshall S. Why Is the Skeleton Still in the Hospital Closet? A Look at the Complex Aetiology of Protein-Energy Malnutrition and Its Implications for the Nutrition Care Team. J Nutr Health Aging. 2018;22(1):26-29. doi: 10.1007/s12603-017-0900-9. PMID: 29300418.
- Quartarolo J, Dolopo A, Richard B. Multidisciplinary effort to improve the diagnosis of malnutrition in hospitalized patients. Nutr Clin Pract. 2021 Oct;36(5):1068-1071. doi: 10.1002/ncp.10644. Epub 2021 Apr 5. PMID: 33821499.
- Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, Kutz A, Tribolet P, Bregenzer T, Braun N, Hoess C, Pavlicek V, Schmid S, Bilz S, Sigrist S, Brändle M, Benz C, Henzen C, Mattmann S, Thomann R, Brand C, Rutishauser J, Aujesky D, Rodondi N, Donzé J, Stanga Z, Mueller B. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet. 2019 Jun 8;393(10188):2312-2321. doi: 10.1016/S0140-6736(18)32776-4. Epub 2019 Apr 25. PMID: 31030981.
- Shepherd E. Malnutrition coding and reimbursement in the hospital setting. Nutr Clin Pract. 2022 Feb;37(1):35-40. doi: 10.1002/ncp.10779. Epub 2021 Sep 29. PMID: 34587310.
- Skipper, A.; Coltman, A.; Tomesko, J.; Charney, P.; Porcari, J.; Piemonte, T.A.; Handu, D.; Cheng, F.W. Reprint of: Position of the Academy of Nutrition and Dietetics: Malnutrition (Undernutrition) Screening Tools for All Adults. J Acad Nut Diet. 2022; 122: S50-S54. doi: 10.1016/j.jand.2022.07.013.
- Sriram K, Sulo S, VanDerBosch G, et al. Nutrition-Focused Quality Improvement Program Results in Significant Readmission and Length of Stay Reductions for Malnourished Surgical Patients. JPEN J Parenter Enteral Nutr. 2018;42(6):1093-1098. doi:10.1002/jpen.1040
- White J V., Guenter P, Jensen G, Malone A, Schofield M. Consensus Statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition. Journal of Parenteral and Enteral Nutrition. 2012;36(3):275-283. doi:10.1177/0148607112440285
- Wills‐Gallagher J, Kerr KW, Macintosh B, Valladares AF, Kilgore KM, Sulo S. Implementation of malnutrition quality improvement reveals opportunities for better nutrition care delivery for hospitalized patients. Journal of Parenteral and Enteral Nutrition. 2022;46(1):243-248. doi:10.1002/jpen.2086 27.
- Sriram K, Sulo S, VanDerBosch G, et al. A comprehensive nutrition-focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. JPEN J Parenter Enteral Nutr. 2017;41(3):384-391.
- Sulo S, Feldstein J, Partridge J, et al. Budget impact of a comprehensive nutrition-focused quality improvement program for malnourished hospitalized patients. Am Health Drug Benefits. 2017;10(5):262- 270.
- Tappenden, KA; Quatrara, B; Parkhurts, M; Malone, A; Fanjiang, G; Ziegler, T. (2013). Critical Role of Nutrition in Improving Quality Care: An Interdisciplinary Call to Action to Address Adult Hospital Malnutrition. J Acad Nutr and Diet. 113 (9); 1219-1237.
- Valladares AF, Kilgore KM, Partridge J, Sulo S, Kerr KW, McCauley S. How a Malnutrition Quality Improvement Initiative Furthers Malnutrition Measurement and Care: Results From a Hospital Learning Collaborative. JPEN J Parenter Enteral Nutr. 2021 Feb;45(2):366-371.